I am scheduled for skin cancer removal. How will my surgeon repair the wound?
A surgical wound (also known as a defect) can be managed in many ways. The choice of management options will vary depending on the body location, size, and depth of the wound, underlying structures, and patient health.
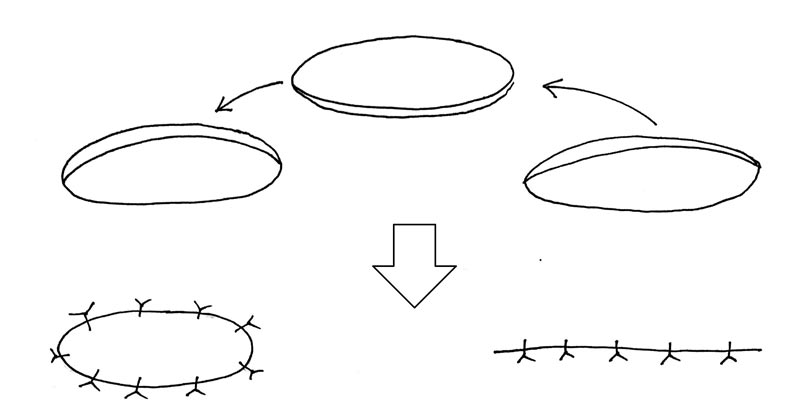
For small and shallow wounds, second intention healing is often used. This simply means allowing the wound to heal on its own. As seen in the image below, a wound healing by second intent both contracts inward (becomes smaller in diameter) and fills in from the bottom up (becomes shallower) with time.
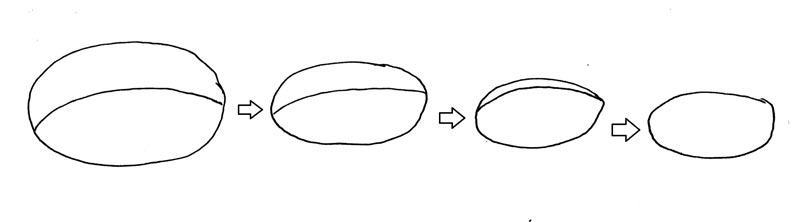 Healing by second intent.
Healing by second intent.Small and simple facial wounds may only require 1-3 weeks to heal by second intent. A large leg wound could take months or even years because the leg has less blood supply than the face, for example. Some sites, such as scalp, have excellent blood supply but may not be good sites for second intent for cosmetic and practical reasons. For example, patients often want to maintain hair density, and hair on the scalp often gets into the wound which disturbs healing.
For larger or deeper surgical wounds, it is often preferable to close the wound, often termed primary intention.
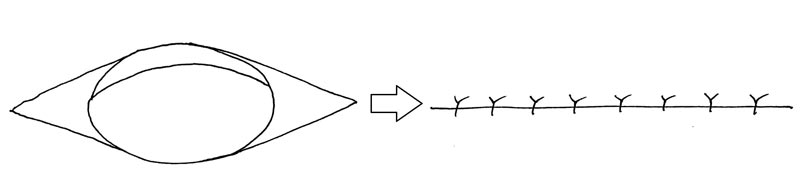 An elliptical wound excision and closure using simple interrupted sutures.
An elliptical wound excision and closure using simple interrupted sutures.The simplest and most effective method of primary wound closure is linear closure. This involves bringing the sides of the wound together which results in a line (hence "linear" closure). In order to prevent bunching at the ends, triangles (often called "dog ears" or Burow's triangles) are sometimes removed (as shown in image). This practice creates a longer scar but lessens the chance of bunching. A 2:1 or 3:1 ratio of length-to-width is usually employed.
A novel method of stretching skin using the SUTUREGARD ISR can be used to limit the removal of these "dog ears". A circular wound (1:1 length-to-width) ratio assumes an approximately 2:1 length-to-width ratio after 30 minutes of SUTUREGARD ISR stretching. This method lessens both bunching of the ends and length of the final scar.
For some wounds, more complex forms of reconstruction can be used. A skin flap involves moving normal skin with an attached blood supply into the wound. Most flaps involve moving local tissue into the wound. Some examples of flaps are shown in the graphics below.
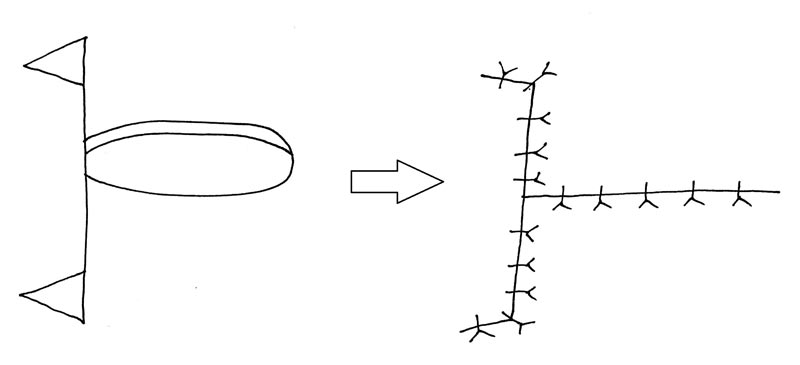 An example of an advancement flap (A-to-T in this case). Notice additional scar lines.
An example of an advancement flap (A-to-T in this case). Notice additional scar lines. 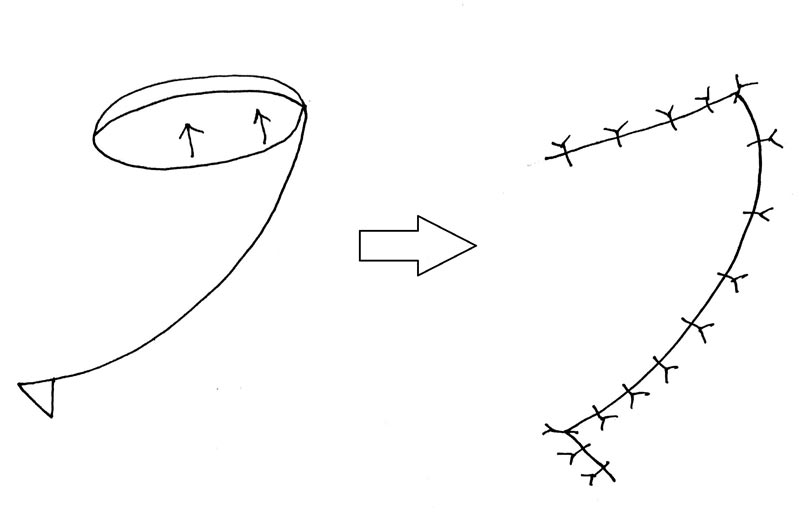 A rotation flap. This would be the most common flap choice for scalp and often requires a scar between 4-6 times as long as the original wound width.
A rotation flap. This would be the most common flap choice for scalp and often requires a scar between 4-6 times as long as the original wound width. 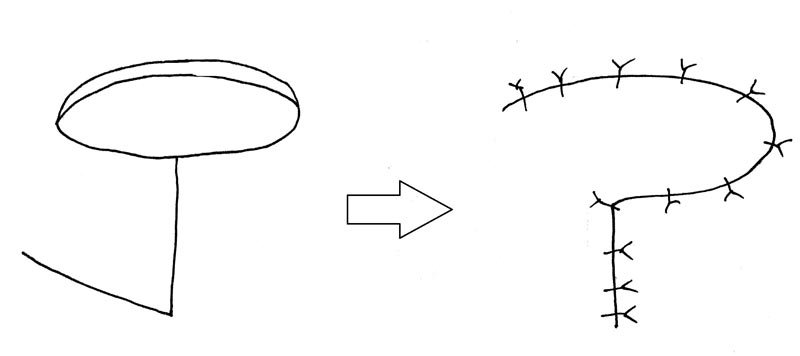 An example of a transposition flap (a Limberg variant of a rhombic flap). Portions of the tip of the flap may receive poor blood supply, so this type of flap is usually only done on the face.
An example of a transposition flap (a Limberg variant of a rhombic flap). Portions of the tip of the flap may receive poor blood supply, so this type of flap is usually only done on the face.In all cases, there are many more lines than would be left by a linear closure. With all flaps, there is also heightened risk that the edges of the flap do not receive adequate blood supply, which will result in wound healing problems. Flaps are also prone to permanent numbness due to cutting nerves to create the flap.
Another option is skin grafting. With grafting, a piece of skin is removed from another body site (donor area) and placed in the wound (recipient area). The donor area is usually closed in a linear fashion or allowed to heal on its own. In contrast to a flap, a skin graft does not have an attached blood supply. Therefore, the graft's survival in the wound relies on the blood supply at the bottom of the wound. Wounds with exposed bone (e.g. skull) or cartilage are poor areas for skin grafting due to poor blood supply.
 Skin grafting involves removing skin from one area and moving it to another area. The graft relies on blood supply from the wound base to survive.
Skin grafting involves removing skin from one area and moving it to another area. The graft relies on blood supply from the wound base to survive.Due to the blood supply issues, skin grafts must be relatively thin and, as a result, can look different than normal skin and have lessened long term sensation. Thinner (split thickness) grafts have a better survival rate than thicker (full thickness) grafts, but generally look worse and have worse final sensation.
For many wounds, skin relaxation with the novel SUTUREGARD® ISR retention suture device method can be used instead of flaps or grafts. Many surgeons in the United States from a variety of subspecialties are currently enjoying the benefits of this procedure in helping reduce the need for flaps and grafts in wound reconstruction.